Many of us are familiar with the occasional twinge or cramp in our lower abdomen, but a sudden, stabbing pain is different. It’s the kind of discomfort that makes you pause and wonder what’s going on inside your body. While it’s easy to brush off pain, this is one signal you shouldn’t ignore. Your body is trying to tell you something, and listening is the first step toward feeling better. This guide is here to help you understand the potential reasons behind that sharp pain and to outline the path toward getting the right sudden stabbing pain in pelvic area female treatment, so you can move from a place of worry to one of informed action and relief.
Key Takeaways
- Get a Clear Diagnosis First: Sharp pelvic pain can stem from many sources, from harmless ovulation to conditions like endometriosis. A professional diagnosis is the only way to identify the root cause and find the right treatment instead of just masking symptoms.
- Know When to Seek Immediate Help: While most pelvic pain isn’t an emergency, sudden and severe pain—especially with a fever or dizziness—requires immediate medical attention. Trust your body’s warning signs and don’t wait to get checked out.
- Create a Comprehensive Relief Plan: Lasting relief often involves more than one solution. A personalized plan may combine medical treatments, specialized pelvic floor therapy, and supportive lifestyle changes to address your specific needs and manage pain effectively.
What’s Causing This Sharp Pelvic Pain?
That sudden, sharp pain in your lower abdomen can be alarming, stopping you right in your tracks. It’s a common experience for many women, but that doesn’t make it any less disruptive. The source of pelvic pain can range from a normal part of your monthly cycle to a sign that something more serious is going on. Understanding the potential causes is the first step toward finding relief and taking control of your health.
Think of your pelvic region as a busy neighborhood—it houses your reproductive organs, bladder, and parts of your digestive system. A problem in any one of these areas can send out a pain signal. Sometimes, the cause is straightforward, like ovulation. Other times, it’s a more complex issue like an infection or a chronic condition. Because the possibilities are so varied, it’s important not to dismiss persistent or severe pain. Getting a clear diagnosis is key to creating an effective pelvic pain treatment plan that addresses the root cause, not just the symptoms.
Common Culprits: Ovarian Cysts and Ovulation
Many women experience a sharp twinge midway through their menstrual cycle, a sensation known as ovulation pain or “mittelschmerz.” This is typically a normal, brief pain that occurs when an ovary releases an egg. Another frequent cause is ovarian cysts, which are fluid-filled sacs that can form on your ovaries. Most are harmless and disappear on their own without you ever knowing they were there. However, if a cyst grows large or ruptures, it can cause a sudden, sharp pain on one side of your pelvis. While often benign, it’s a good idea to have any persistent pain evaluated by a doctor.
Conditions Like Endometriosis and Adenomyosis
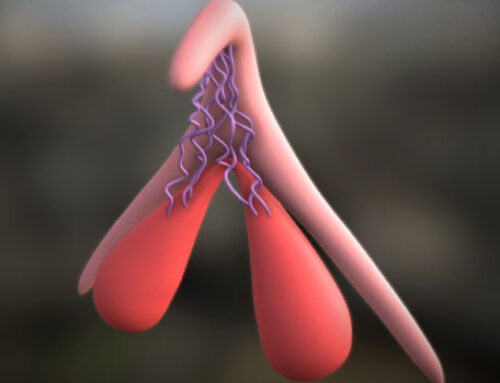
If you experience severe, stabbing pain, especially around your period, it could be related to a condition like endometriosis. This happens when tissue similar to the uterine lining grows outside the uterus, often on the ovaries or fallopian tubes. This misplaced tissue responds to hormonal changes, leading to inflammation, scarring, and intense pain. Adenomyosis is a similar condition where the tissue grows into the muscular wall of the uterus itself, causing heavy periods and severe cramping. Both conditions can significantly impact your quality of life, but effective treatments are available to manage the symptoms.
Infections and Inflammatory Diseases
Sometimes, that sharp pain is your body’s alarm system signaling an infection. Pelvic inflammatory disease (PID) is a serious infection of the reproductive organs, often stemming from an untreated STI. It can cause sharp pain, fever, and unusual discharge. Urinary tract infections (UTIs) are another common source of pelvic discomfort, though the pain is often accompanied by a burning sensation during urination and a frequent urge to go. It’s crucial to treat these infections promptly to prevent them from causing more serious, long-term health problems. Our clinic offers comprehensive care for your sexual and urinary tract health.
Urgent Issues: Ectopic Pregnancy and Ovarian Torsion
While most pelvic pain isn’t an emergency, some causes require immediate medical attention. An ectopic pregnancy, where a fertilized egg implants outside the uterus (usually in a fallopian tube), can cause sharp, one-sided pain and is life-threatening if not treated. Another emergency is ovarian torsion, which occurs when an ovary twists around its supporting ligaments, cutting off its blood supply. This causes sudden, severe pain, often with nausea and vomiting. If you experience excruciating pain, especially with dizziness or fever, head to the nearest emergency room right away. These are serious medical conditions that need immediate intervention.
Bladder and Urinary Tract Problems
Your bladder can also be the source of sharp pelvic pain. Interstitial cystitis, also known as painful bladder syndrome, is a chronic condition that causes bladder pressure, pain, and a persistent, urgent need to urinate. The pain can range from a dull ache to sharp, stabbing sensations in the pelvic area. Unlike a UTI, it isn’t caused by an infection, and the symptoms can flare up in response to certain triggers like stress or specific foods. If you’re dealing with bladder-related pain or incontinence, specialized treatments can help manage your symptoms and restore your comfort.
Is It an Emergency? When to Get Help Now
It can be tough to know when pelvic pain is just a nuisance and when it’s a sign of something more serious. While many causes of pelvic pain can be managed with your doctor’s guidance, some situations require immediate medical care. Trust your instincts—if the pain feels severe or wrong, it’s always best to get it checked out. Understanding the difference between discomfort and a true emergency can help you make the right call for your health and get the care you need without delay.
Warning Signs That Require Immediate Attention
Think of sudden, sharp, and severe pelvic pain as your body’s emergency alert system. This isn’t the kind of pain you should try to wait out. If you experience a stabbing pain that comes on abruptly and is so intense it makes you double over, it’s time to get medical help right away. This is especially true if the pain doesn’t improve with rest or over-the-counter pain medication. Severe pain could signal a serious issue like an ectopic pregnancy or ovarian torsion, where timely treatment is critical. Don’t hesitate to go to an urgent care center or the emergency room.
Red Flag Symptoms You Shouldn’t Ignore
Beyond sudden, severe pain, there are other red flag symptoms that warrant a prompt call to your doctor. Pay close attention if your pelvic pain is accompanied by a fever, chills, or feeling faint. You should also seek care if you notice unusual vaginal discharge or bleeding, blood in your urine or stool, or if it suddenly becomes difficult or painful to urinate. According to the Cleveland Clinic, you should also see a doctor if the pain is new, gets worse over time, or starts to interfere with your daily activities. If you are pregnant, any persistent pelvic pain that doesn’t ease up when you rest or change positions should be discussed with your provider immediately.
How to Find Relief at Home
When you’re hit with sudden pelvic pain, your first thought is likely, “How do I make this stop?” While it’s crucial to get a proper diagnosis from a healthcare professional to address the root cause, there are several things you can do at home to manage the discomfort in the meantime. These simple strategies can help soothe your symptoms and provide temporary relief while you figure out your next steps. Think of them as your first-aid kit for pelvic pain—supportive measures to help you feel more comfortable in your own body. Remember, these tips are for managing mild, temporary pain; severe or persistent pain always warrants a call to your doctor.
Using Over-the-Counter Pain Relievers
For many types of pelvic pain, an over-the-counter (OTC) pain reliever can be a good first line of defense. Medications like ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) are often effective at taking the edge off. Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that works by reducing inflammation, which can be a source of pain. Acetaminophen works differently, by changing the way your body senses pain. Following the dosage instructions on the package is key. While these medications can provide temporary relief from pain, they aren’t a long-term solution and won’t fix the underlying issue.
The Power of Heat and Gentle Movement
Never underestimate the comforting power of warmth. Applying a heating pad or a warm compress to your lower abdomen can work wonders by helping to relax tense pelvic muscles. A warm bath can have a similar soothing effect, easing cramps and overall discomfort. While it might feel counterintuitive to move when you’re in pain, gentle activity can also be incredibly helpful. Light stretching or a slow walk can increase blood flow to the pelvic region, which helps reduce tension and stiffness. The key is to listen to your body and stick to movements that feel good, not forced. For persistent issues, a professional pelvic pain treatment plan is essential.
Why Hydration and Rest Are Key
Sometimes the simplest remedies are the most effective. Staying well-hydrated is important for your overall health, and it can play a role in preventing muscle cramps and spasms that contribute to pelvic pain. Make sure you’re sipping water throughout the day. Just as important is giving your body adequate rest. When you’re dealing with pain, your body is working hard to manage it and heal. Allowing yourself to rest—whether that means taking a nap, going to bed early, or just relaxing on the couch—gives your body the chance to recover. It’s a fundamental part of self-care that supports your body’s natural healing processes.
How Your Doctor Will Diagnose Pelvic Pain
Finding the source of sharp pelvic pain can feel like a mystery, but it’s one your doctor is trained to solve. Think of the diagnostic process as a careful, step-by-step investigation designed to uncover the root cause of your discomfort, not just mask the symptoms. It all starts with a conversation. By listening to your unique experience and understanding your health background, your doctor can begin to connect the dots and narrow down the possibilities. This initial discussion is followed by a physical exam, which allows your doctor to check for any immediate signs of what might be wrong. It’s a collaborative process where your input is the most valuable piece of the puzzle.
Depending on what this initial evaluation reveals, your doctor may recommend further tests to get a clearer picture of what’s happening inside your body. This thorough approach is crucial because so many different conditions can cause pelvic pain, from hormonal imbalances to structural issues. The goal is to move beyond guesswork and get a precise diagnosis. This is the most important step toward creating a personalized pelvic pain treatment plan that addresses the specific source of your pain and brings you lasting relief. It’s all about getting the right answers so you can get the right care.
The Initial Exam and Your Health History
Your first appointment is all about gathering information. Your doctor will start by asking detailed questions about your health history and the specific symptoms you’re experiencing. Be prepared to talk about your menstrual cycle, sexual health, any past pregnancies or surgeries, and the nature of your pain—is it constant or does it come and go? Where exactly do you feel it? What makes it better or worse? The more details you can provide, the better. This conversation is followed by a physical exam, which will likely include a pelvic exam, to check for any tenderness, lumps, or other abnormalities.
Using Imaging and Lab Tests to Get Answers
If your health history and physical exam don’t provide a clear answer, your doctor will likely recommend some tests to look deeper. These aren’t just random checks; each one is chosen to rule out or confirm specific conditions. Lab work, such as blood and urine tests, can identify signs of infection, inflammation, or hormonal issues, which are all key aspects of your overall sexual & urinary tract health. An ultrasound is often a next step, as it uses sound waves to create images of your pelvic organs, helping to spot things like cysts or fibroids. In some cases, more detailed imaging like a CT scan or MRI might be used to get an even clearer view of the area.
Exploring Medical Treatments for Pelvic Pain
When home remedies aren’t cutting it, it’s time to explore medical treatments that can offer more significant and lasting relief. The right approach depends entirely on what’s causing your pain, which is why a thorough diagnosis is the first and most important step. Once your doctor identifies the root cause, they can create a personalized treatment plan that might include hormone therapy, targeted medications, or even minimally invasive procedures.
Balancing Hormones with Bioidentical Therapy
Hormones are powerful, and when they’re out of sync, they can contribute to issues like pelvic pain. This is especially common during perimenopause and menopause, when declining estrogen leads to conditions like vaginal atrophy and dryness that cause discomfort. If a hormonal imbalance is a factor, your doctor might suggest hormone treatments. Bioidentical Hormone Replacement Therapy (BHRT) is a fantastic option because it uses hormones structurally identical to the ones your body produces, offering a natural approach to restoring balance and alleviating symptoms.
Prescription Medications for Pain Relief
Sometimes, targeted medication is the most direct path to relief. Depending on the diagnosis, your doctor may prescribe something stronger or more specific than over-the-counter pain relievers. This could include medications that target nerve pain, muscle relaxants to ease severe cramping and tension in the pelvic floor, or anti-inflammatory drugs. If an underlying infection is the cause, a course of antibiotics will be prescribed to clear it up. These medications are often part of a broader pelvic pain treatment plan that addresses the root cause while managing your immediate discomfort.
Advanced, Minimally Invasive Procedures
If your pain is linked to a structural issue or doesn’t respond to other treatments, your doctor may recommend an advanced procedure. Don’t worry—many of today’s options are minimally invasive with little downtime. Treatments like Votiva use gentle radiofrequency energy to address issues like vaginal laxity and painful intercourse. These innovative procedures can resolve underlying problems that cause chronic pain, offering a long-term solution when other methods fall short. A thorough evaluation will determine if you are a candidate for one of these therapies.
How Pelvic Floor Therapy Can Help
When you hear the term “pelvic floor therapy,” you might immediately think of Kegels. But this specialized physical therapy goes far beyond a single exercise. Your pelvic floor is a complex network of muscles that supports your bladder, uterus, and bowels. When these muscles are too tight, too weak, or uncoordinated, they can become a major source of sharp, stabbing pain. Pelvic floor therapy is a hands-on, personalized approach that gets to the root of these muscular issues.
A trained therapist can identify exactly what’s causing your discomfort—whether it’s muscle spasms, trigger points, or weakness—and create a plan to address it. This isn’t about pushing through the pain; it’s about retraining your body to function correctly and without discomfort. For many women, it’s a critical component of a comprehensive pelvic pain treatment plan. By focusing on the muscular system that underpins your entire core, this therapy can provide lasting relief and help you feel more in control of your body.
The Benefits of Strengthening Your Pelvic Floor
A strong and well-coordinated pelvic floor is fundamental to your overall well-being. These muscles act as a supportive sling for your pelvic organs, and when they’re functioning properly, they can significantly reduce or even eliminate pain. Pelvic rehabilitation, a focused type of physical therapy, is proven to help manage and reduce pelvic pain by restoring balance to this crucial area. The benefits often extend beyond pain relief, leading to better bladder control and a reduction in issues like stress incontinence. By strengthening and coordinating these muscles, you’re not just treating a symptom; you’re building a stronger foundation for your core health.
Targeted Exercises and Manual Therapy
Pelvic floor therapy is not a one-size-fits-all solution. A specialist will begin with a thorough evaluation to understand your unique muscle patterns. This often includes manual therapy, where the therapist uses hands-on techniques to release tight tissues, break up scar tissue, and reduce inflammation. From there, they will guide you through therapeutic exercises tailored to your specific needs. These might include stretches to relax tense muscles, stability exercises to improve posture, or strengthening movements using tools like V Tone to gently stimulate and tone weak muscles. This targeted approach ensures you’re working on the right things to find effective relief.
Relaxation Techniques and Biofeedback
Sometimes, pelvic pain isn’t caused by weakness but by muscles that are constantly clenched and overworked. You may not even be aware that you’re holding this tension. Relaxation techniques are designed to help you release this chronic tightness. One of the most effective tools for this is biofeedback, a method that helps you become aware of your body’s subtle signals. Using small sensors, biofeedback gives you real-time information about muscle tension, allowing you to consciously learn how to relax those muscles on command. Mastering this skill is incredibly empowering and can make all other therapies more effective, giving you a powerful tool to manage pain long-term.
Complementary Approaches to Manage Pain
While medical treatments are essential for getting to the root cause of pelvic pain, a truly comprehensive approach to wellness often includes strategies that support your whole body. Think of these complementary methods not as replacements for your doctor’s care, but as powerful allies that work alongside your treatment plan. They can help manage symptoms, reduce the heavy stress that often comes with chronic pain, and give you a greater sense of control over your health and your life. When you’re dealing with sudden, sharp pain, it’s easy to feel like your body is working against you. Integrating practices that calm your nervous system and reduce inflammation can completely shift that dynamic.
By looking beyond conventional medicine, you can build a personalized toolkit for managing pain that addresses both your physical and emotional well-being. This might include anything from acupuncture to specific dietary changes. The goal is to create a supportive lifestyle that helps you feel better day-to-day. Working with a specialist like Dr. Berman ensures that any complementary therapies you explore are a safe and effective part of your overall pelvic pain treatment plan. This holistic view empowers you to take an active role in your healing journey, creating a sustainable path toward feeling your best.
Mind-Body Practices Like Acupuncture
If you’ve never tried acupuncture, the idea of needles might seem intimidating, but it’s a gentle and widely recognized practice for pain management. It involves placing hair-thin needles at specific points on the body to help restore balance and flow. For pelvic pain, this ancient technique is thought to work by stimulating nerves and encouraging your body to release endorphins—its own natural pain-relieving chemicals. Many women find that regular acupuncture sessions can significantly reduce the intensity and frequency of sharp pelvic pain, offering a calming and restorative way to manage their symptoms without medication.
How Diet and Stress Management Make a Difference
The connection between your mind, your gut, and pain is incredibly strong. When you’re under constant stress, your body can become more sensitive to pain signals. Simple mind-body practices like meditation, gentle yoga, or even just a few minutes of deep breathing can help calm your nervous system and lower your perception of pain. At the same time, what you eat matters. Certain foods can contribute to inflammation, which is often a key driver of pain. Focusing on an anti-inflammatory diet rich in leafy greens, berries, fatty fish, and nuts can help soothe your system from the inside out. These lifestyle adjustments are powerful tools for long-term wellness and pain management.
Understanding When Surgery Is an Option
If you’ve tried other treatments without finding the relief you need, the idea of surgery might come up. I know that can sound intimidating, but it’s important to know that when it comes to pelvic pain, surgery is often a highly effective solution for specific underlying issues. It’s a path we consider when we can pinpoint a structural cause for your pain that can be corrected, finally offering you a chance at long-term comfort.
The decision to have surgery is always a conversation between you and your doctor, focused entirely on your health and quality of life. The great news is that many modern procedures are minimally invasive. This means smaller incisions, less discomfort, and a much quicker return to your daily routine compared to traditional surgeries of the past. When other options haven’t worked, surgery can be the definitive step toward resolving the root cause of sudden, stabbing pelvic pain and helping you feel like yourself again.
Exploring Surgical Treatments
Surgery is typically recommended when your pelvic pain is caused by a specific, identifiable condition. Doctors may suggest surgery for pelvic pain to address issues like endometriosis, uterine fibroids, or ovarian cysts that are causing significant problems. The goal is to remove the problematic tissue or cysts that are triggering the pain signals.
Many of these procedures are performed using minimally invasive techniques, such as laparoscopy. This involves making a few small incisions and using a tiny camera to see inside the pelvic area, allowing for precise treatment without a large opening. This approach is gentler on the body, leading to less post-operative pain and a faster recovery.
What to Expect During Recovery
Your recovery journey will depend on the exact type of surgery you have. One of the biggest benefits of minimally invasive procedures is that the recovery period is generally much shorter and more comfortable than with traditional open surgery. You can expect some discomfort in the days following the procedure, but your doctor will create a plan to manage it effectively with medication.
Following your post-operative care instructions is the most important thing you can do to ensure a smooth and speedy recovery. This includes getting enough rest, following guidelines on physical activity, and attending your follow-up appointments. Open communication with your care team will help you feel supported as you heal and get back to living without pain.
Preventing Pelvic Pain in the Future
Once you have a diagnosis and a treatment plan, the next step is looking ahead. Taking proactive steps can help you manage your pelvic health and reduce the chances of pain returning. It’s all about creating a foundation for long-term wellness and staying in tune with your body. By focusing on sustainable habits and consistent medical care, you can feel more in control of your health and well-being. This approach isn’t about a quick fix; it’s about building a lifestyle that supports you for years to come.
Lifestyle Changes for Long-Term Wellness
It’s amazing how much our daily habits influence our pelvic health. Simple, consistent changes can make a world of difference in preventing future pain. For instance, regular exercise is fantastic for increasing blood flow and can help reduce your risk of pelvic pain. If you smoke, consider this another great reason to quit, as tobacco can lead to nerve inflammation that makes pain worse. And since stress is a known contributor to pelvic discomfort, finding ways to unwind is key. Incorporating relaxation techniques like yoga or meditation into your routine can significantly lower stress levels and support your overall well-being.
The Importance of Regular Health Check-ups
Staying on top of your health is one of the most powerful things you can do. Regular check-ups with your healthcare provider are essential for early detection and management of potential issues that could lead to pelvic pain. It’s so important to listen to your body. If you experience new pelvic pain that interferes with daily activities or worsens over time, it is important to consult a healthcare professional. You should always seek medical advice if your pain is persistent or severe, as timely intervention can prevent complications. Your health is a priority, and you should never hesitate to reach out for support.
Questions to Ask Your Doctor About Pelvic Pain
Walking into your doctor’s office prepared can make all the difference. Since so many different conditions can cause pelvic pain, trying to figure it out on your own isn’t the best path forward. A conversation with a healthcare provider is the first step toward getting the right diagnosis and, more importantly, the right treatment. Feeling ready for that conversation can help you advocate for your health and ensure all your concerns are addressed.
Think of this appointment as a fact-finding mission. Your goal is to give your doctor a clear picture of what you’re experiencing and to leave with a clear understanding of the next steps. Don’t hesitate to bring a list of questions with you. Some good starting points include: What are the possible causes of my pain? What tests will I need to get a diagnosis? What are my treatment options, and what are the pros and cons of each? This proactive approach helps you become an active partner in your own healthcare journey.
How to Prepare for Your Appointment
To get the most out of your visit, take some time to think through your symptoms. Your doctor will want to know about your health history, so be ready to share as much detail as you can. When did the pain start? Is it constant or does it come and go? What does it feel like—sharp, dull, cramping? Does anything make it better or worse? Your doctor will perform a physical exam and may recommend tests like blood work, an ultrasound, or an MRI to get a clearer picture. The more information you can provide, the easier it will be to pinpoint the cause and find an effective pelvic pain treatment.
Making Sense of Your Treatment Plan
Once your doctor has a better idea of what’s causing the pain, you can discuss a treatment plan. This plan will be tailored specifically to you. Depending on the diagnosis, your doctor might suggest a range of options. For infections, antibiotics are a common solution. For pain management, they might recommend specific painkillers or hormone treatments to address underlying imbalances. In many cases, physical therapy designed to relax and strengthen the pelvic floor muscles can provide significant relief. Dr. Berman offers a variety of advanced services that can be integrated into a comprehensive and personalized plan to help you feel your best.
Related Articles
- The Use of Physical Therapy in Treatment for Endometriosis | Dr. Jennifer Berman MD
- Endometriosis Awareness: Insights and Treatments
- Pelvic Pain Treatment Beverly Hills & Santa Monica | Dr. Jennifer Berman MD
- Pleasure or Pain Sex: Why It Hurts & How to Fix It
- Emsella Chair Reviews: What to Know Before You Buy
Frequently Asked Questions
How can I tell the difference between normal cycle pain and something more serious? This is a great question because it gets to the heart of the anxiety so many of us feel. Think about patterns. Normal pain related to your cycle, like ovulation twinges or cramps, is usually predictable. It happens around the same time each month, feels familiar, and typically eases up with a heating pad or an over-the-counter pain reliever. Pain that signals a more serious issue often breaks that pattern. It might be sudden and severe, stick around long after your period ends, or come with other red flag symptoms like a fever, dizziness, or unusual bleeding.
Can stress alone really cause sharp pelvic pain? Absolutely. Your mind and body are deeply connected, and stress is notorious for causing physical symptoms. When you’re stressed, your body tenses up, and that includes the complex network of muscles in your pelvic floor. Chronically tight pelvic muscles can lead to spasms, trigger points, and sharp, stabbing pains. While stress might not be the cause of something like an ovarian cyst, it can certainly make existing pain feel much worse or be a primary driver of muscle-related pelvic pain on its own.
I’ve been told to just do Kegels. Is pelvic floor therapy different? Yes, it’s very different, and this is a crucial distinction. Kegels are an exercise designed to strengthen the pelvic floor muscles, which is helpful if your issue is weakness. However, many women with pelvic pain actually have muscles that are too tight, or “hypertonic.” In that case, doing Kegels can make the pain worse. A pelvic floor therapist provides a complete evaluation to figure out exactly what your muscles need—whether that’s strengthening, relaxation, or coordination—and creates a personalized plan with manual therapy and targeted exercises that go far beyond Kegels.
If my doctor can’t find anything on an ultrasound, does that mean the pain is all in my head? Not at all. Your pain is real, and a clear ultrasound is actually a valuable piece of information, not a dead end. An ultrasound is excellent for looking at the structure of your organs, like your uterus and ovaries, to rule out things like large cysts or fibroids. However, it can’t show everything. It won’t reveal muscle tension, nerve irritation, or conditions like interstitial cystitis. A normal scan simply means you and your doctor can cross a few things off the list and look deeper into other potential causes.
What kind of doctor should I see for this type of pain? Starting with your primary care doctor or gynecologist is always a good first step. They can rule out common issues and infections. However, if your pain is persistent, severe, or your doctor has trouble finding a clear cause, it’s time to see a specialist. A physician who focuses on women’s sexual health and pelvic disorders, like Dr. Berman, has the advanced training and diagnostic tools to investigate complex cases and offer a wider range of specialized treatments that a general practitioner might not.